Something Smells Bad
How to Avoid Food PoisoningWe see advertising actually creating and naming taboos. - Howard Luck Gossage
by David Schardt & Stephen Schmidt "I want to tell you about what it's like to survive a severe attack of Salmonella, because there are too many people who have died and can't tell you what it is like. I got Salmonella from something I ate. The most likely culprits are a chicken sandwich and an undercooked egg salad sandwich. I first got diarrhoea which lasted for days and days. Then quite suddenly, the diarrhœa stopped. Soon I felt as if there was a red hot brick inside me. It was the most awful thing I had ever experienced. I knew that I had to go to the hospital. And I knew that I was going to need surgery to live..." Washington, DC, businessman Bill Adler, Jr. almost died in 1990 after eating Salmonella-contaminated food. "Fifty-five thousand dollars later, I'm as healthy as I was before this happened," he says. The only casualties: the colostomy he had for nearly a year and the four inches that were cut from his colon. Adler was lucky. He lived. Twenty-five Americans will die today - and another 16,000 will become ill - from something they ate. Here are the foods that are most likely to make you sick. (The list doesn't include seafood.) Chicken and TurkeyRussian roulette. If you're among the most susceptible, one out of every four chickens - and one out of every seven turkeys - has enough Salmonella to make you sick... or kill you. It's that simple. And while cooking destroys the bacteria, that message doesn't always get through. The US Department of Agriculture estimates that anywhere from 350,000 to 2.5 million Americans are taken ill - and 350 to 2,500 die - every year after eating Salmonella-contaminated poultry and meat (about 1% of all cattle is also infected). The estimates are so broad because most food poisoning cases are never reported to health authorities. "For every one we hear about, there are 20 to 100 that go unreported," says Tom Gomez, a USDA epidemiologist at the Centers for Disease Control (CDC) in Atlanta. Poultry producers don't deny that at least a quarter of the chickens they send to market carry dangerous bacteria. But they downplay the risk. "Ninety percent of chickens found with Salmonella have fewer than 30 bacteria on the whole bird," says Kenneth May, the scientific advisor for the industry's National Broiler Council. "Thirty bacteria probably won't make you sick if you're a healthy person in the prime of your life," agrees Gomez. "But it could if you're one of those most susceptible to food poisoning." Like children. In 1994, the Schwan's Ice Cream that made an estimated 224,000 people sick (most of them were youngsters) contained only six Salmonella bacteria per half cup. (One of the ice cream's ingredients had been transported in tanker trucks that had previously carried contaminated raw eggs.) Is skinless, kosher, or "free-range" chicken any less likely to be contaminated? No good studies have been done. And that's for the best-studied bacterium. Others - Campylobacter, for example - aren't being monitored as closely. "Campylobacter causes more illnesses than Salmonella, though it doesn't get as much notoriety," says Gomez. "It should." In other words, chalk up another two million or so illnesses every year... and who knows how many deaths. The problem, says Gomez, is that "local diagnostic labs don't test for Campylobacter, and state health departments aren't required to report it to the CDC. They should." Based on the results of a pilot surveillance program, CDC Director David Satcher was able to tell a congressional committee in May that Campylobacter is "the most frequently isolated foodborne bacterium from persons with diarrhœa." Not too comforting. EggsHow many people were felled last year by contaminated eggs? Nobody knows. "We have incomplete data after 1994," says the CDC's Tom Gomez. Congress is to blame, at least in part. In 1995, in the name of cost-cutting, it terminated the federal control program for Salmonella enteritis (EN-terr-ID-iss); enteritis is the strain of Salmonella that's most likely to affect eggs. But there's no reason to think that 1995 or 1996 is any different than 1994, when Americans probably suffered from "between 200,000 and 1,000,000 actual infections" caused by Salmonella enteritis, CDC Director Satcher testified in May. The culprit? "Shell eggs accounted for 80% of those outbreaks for which a vehicle was determined," said Satcher. Even scarier: Most tainted eggs are contaminated within the hens' ovaries before their shells form. So washing the eggs before cracking them open is no guarantee that they'll be clean. While no deaths from outbreaks caused by Salmonella-contaminated eggs were reported to federal authorities in 1994, disease-control experts remain concerned. "The big news is that the number of infections has tripled in Southern California," says CDC epidemiologist David Swerdlow, who adds that California now accounts for about 25% of all Salmonella infections in the country. What's more, most of the Southern California infections are due to a new, worrisome form of Salmonella enteritis called "phage type 4." (Bacteria can be distinguished from one another by the phages, or viruses, that infect them.) "Phage type 4 has been a more virulent form of Salmonella in Europe, but we don't know yet whether that will also be true in the United States," says Richard Gast, a microbiologist at the US Department of Agriculture's Southern Poultry Research Laboratory in Athens, Georgia. "So far, we haven't been able to determine in the lab whether it's a nastier bacteria. If we can't, we may be reduced to watching what happens in the western United States." Phage type 4 has now also been detected in Utah and Arizona. So who's minding the egg carton? Nobody. There is no nationwide program that systematically monitors bacteria levels in eggs. But a new USDA survey suggests that the rate may be rising. "Our analysis of eggs sent to processing plants for pasteurisation in the Northeast showed that 39% of the samples were contaminated with Salmonella enteritis in 1995, compared with 20% in 1991," says USDA animal scientist Allan T Hogue. "And in the West," he adds, "12% were contaminated in 1995 versus 6% in 1991." Many restaurants - and most high-risk sites like hospitals and nursing homes-use pasteurised eggs because the process kills disease-causing bacteria. Unfortunately, nobody knows whether the high rate of Salmonella contamination of eggs destined for pasteurisation applies to the eggs sold in local supermarkets. BeefRemember E coli O157:H7? That's the bug that made more than 700 people ill - and sent four children to their graves - in 1993 in Washington State, California, Idaho, and Nevada. The source was undercooked fast food hamburgers. E coli O157:H7 does its damage by producing a substance called "Shiga toxin," which causes the bloody diarrhoea that strikes most victims. "The toxin leads to kidney failure in about 5% of the victims, and then death in about 5% of those whose kidneys fail," says microbiologist David Acheson of the New England Medical Centre in Boston. Since cooking beef to 165oF kills the bacteria, E coli on the surface of steaks and roasts is easily destroyed, even if they're eaten rare. But when raw beef is ground up, any bacteria on its surface can become incorporated into the mix. If the burger isn't cooked thoroughly, the E coli that's on the inside can escape destruction. And escape destruction is what O157:H7 bacteria continue to do. "In 1994 and 1995, 64 more outbreaks involving about 1,000 people - but no deaths - were reported to us," says Phyllis Sparling, a USDA epidemiologist at the CDC. The real toll is probably far higher. That's because the CDC numbers only count outbreaks, which involve two or more people who become sick from the same food. Individual cases aren't included in the official tally. So the CDC never knew about the death last year of two-year-old Elizabeth Paige Hall, for example. The toddler died at the Cleveland Clinic Hospital four weeks after attending a cookout at which she ate a tainted hot dog. It picked up the O157:H7 from raw hamburger meat that had sat on the same plate. After the 1993 outbreaks, the USDA started regularly testing raw ground beef for bacterial contamination. "Each year, we analyse about 5,000 samples of ground beef from retail stores and processing plants for the presence of E coli O157:H7," says Glenn Morris, director of epidemiology and emergency response at the USDA's Food Safety and Inspection Service (FSIS). "Since 1994," he adds, "only about one in 1,700 samples has tested positive." That's good, but it may lull authorities into a false sense of security. A new study concludes that O157:H7 may not be the only culprit. When David Acheson analysed ground beef from 12 supermarkets in Boston and Cincinnati, he found Shiga toxin in a quarter of the samples. "Even more alarming," he says, "is that none of the toxin came from E coli O157:H7. It was all produced by other kinds of E coli. That has huge implications, because the USDA only looks for E coli O157:H7 in ground beef." "The other E coli could be responsible for up to half the cases of bloody diarrhoea and kidney failure caused by Shiga toxin in North America," says Mohammed Karmali, a microbiologist at the Hospital for Sick Children in Toronto. And nobody's looking for those other bacteria in ground beef. That needs to change. When to Get HelpFood poisoning usually involves nausea, vomiting, or diarrhoea. Most cases clear up by themselves within a day or two without medical care. But if you get any of these symptoms, says infectious diseases specialist William Bishai of the Johns Hopkins School of Public Health, you need to call the doctor:
If you get food poisoning, report it to your local health department. That's the only way to get it into the official count. Who's Most Vulnerable?"Some people are more likely to get food poisoning and more likely to come down with a bad case of it," says William Bishai of the Johns Hopkins School of Public Health:
Duel of the Cutting BoardsWhich is safer: wooden or plastic cutting boards? Until 1993, the conventional wisdom was that plastic was easier to keep free of bacteria. Then along came Dean Cliver of the University of Wisconsin at Madison. The microbiologist smeared nine wooden and four plastic boards with chicken juice or broth that he had spiked with E coli, Listeria, or Salmonella. Then he waited. After three minutes, the surfaces of the plastic boards had up to 23 times more bacteria than the surfaces of the wooden boards. More amazingly, within 10 minutes the wooden boards had completely absorbed the bacteria, and Cliver couldn't recover them. "On wooden boards, bacteria are absorbed down into the wood fibre and remain beneath the surface," Cliver explains. "On plastic boards they cling to the surface, where they can more easily rub off onto other objects like food." In 1994, Food and Drug Administration microbiologist Ben Tall weighed in with his own cutting board study. "Wood seems to be more forgiving, in that the bugs get down deep and it's probably harder for them to come back out," agrees Tall. But that was only true of new wooden boards, or of "freshly cleaned" boards that had been sanitised through a dishwasher. "A used wooden cutting board, which is what most people have in their homes," he adds, "probably would act more like a plastic board." In other words, it would be more likely to spread bacteria. Until the question is settled, the best advice is to use either kind of board... as long as you keep it clean. "If you put a wood board in the microwave for five minutes, you'll even kill the bacteria that are lurking deep inside," says Cliver. As for plastic, "If it's knife-scarred," says Cliver, "the only effective way to clean it is in the dishwasher. It doesn't get hot enough in the microwave." And if any board really gets hacked up, toss it. The Safe Food KitchenEight tips to make your kitchen safer:
Where to Get Help
Source: I downloaded this off the Web several years ago and saved it because I thought it contained information I needed to know. I no longer know the exact source; if anyone reading this knows, please contact me.
How to Wash Hands Properlyby Centers for Disease Control and the American Society for Microbiology Washing hands to prevent infection entails more than a quick splash under the faucet. Here's how to wash hands properly, to prevent the spread of colds and other respiratory viruses:
How to wash with hand sanitizer:
Source: ohio.com 20 January 2004
Office Dirtby April Umminger and Sam Ward
Source: Microbiologist Sam Gerba, University of Arizona via USA Today 10 June 2002
Sweating and Body OdourSweating is your body's normal response to the buildup of body heat. Sweating varies widely from person to person. Many women perspire more heavily during menopause. Drinking hot beverages, or those containing alcohol or caffeine, can cause temporary increases in sweating. For most people, sweating is only a minor nuisance. But for some people, sweaty armpits, feet and hands are a major dilemma. Sweat is basically odourless, but it may take on an unpleasant or offensive odour when bacteria multiply and break down the body's secretions into odour-causing by-products. Mood, activity, hormones and some foods, such as caffeine, may influence sweating and odour. A "cold sweat" is usually the body's response to a serious illness, anxiety or severe pain. Seek immediate medical attention for a "cold sweat" if you have signs of light-headedness or chest and stomach pains.
Your doctor may recommend a prescription antiperspirant. For a few people, surgery may help. The operation removes the troublesome sweat glands. However, this is appropriate for only a few people who have persistent soreness and irritation caused by antiperspirants or excessive sweating. Consult your doctor if there's an increase in sweating or nighttime sweating without an obvious cause. Infections, thyroid gland dysfunction and certain forms of cancer may produce unusual sweating patterns. Excessive sweating associated with shortness of breath requires immediate action. This could be a sign of a heart attack. Occasionally, a change in odour signals a disease. A fruity smell may be a sign of diabetes, or an ammonia-like smell could be a sign of liver disease. Source: www.walgreens.com 25 October 1999 from the Mayo Clinic
What to Do about Smelly FeetIs someone baking cheese in here?! If your feet warp steel every time you take off your sneakers, thank an overgrowth of bacteria or fungus. "The hotter and moister the foot is in the shoe, the more your feet will sweat, which means more bacteria will multiply and cause offensive odours," explains Janice Steinberg, MD, a Ft Lauderdale-based dermatologist. But this doesn't mean you're consigned to wearing hippie-type Birkenstocks. Just take these reek-busting steps. First, eliminate the bacteria-breeding environment by tossing out your oldest shoes. Wear only loose-fitting ones, alternating pairs each day to cut down on bacteria growth and give your shoes time to air out. Sprinkle some destenchifying powder inside your shoes daily. Stick to cotton socks, which absorb the sweat bacteria thrive in. Finally, make sure you park your hooves under the bathtub faucet twice each day and give them a good scrubbing with soap. Lather up between toes (bacteria love to take up residence in these crevices) and thoroughly dry each foot before putting your socks on. And no grape stomping until the air clears up in here, capiche? Source: Maxim May 2001
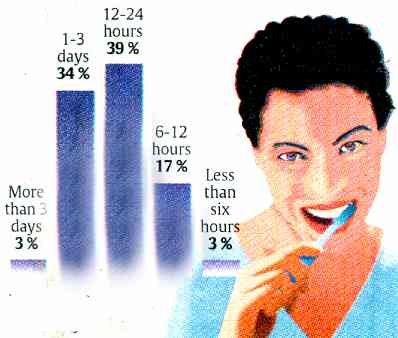
Bad Breathby Mike Spector and Bob Laird How long has it been since you brushed your teeth?
Source: Impulse Research Corporation for the Mentadent Smart Mouth Survey via USA Today 10 June 2002
Oral Health in America: A Report of the Surgeon General confirms that signs of life-threatening diseases appear in the mouth before they show up in other parts of the body. Dentists routinely look for symptoms of oral cancer, diabetes, eating disorders and HIV, which can be detected during regular examinations. Detecting disease early is key to saving lives. The presence of gum disease has been linked to the development of heart disease, respiratory ailments, and the delivery of pre-term low birth weight babies. A primary bacteria found in the mouth when gum disease is present can enter the blood stream and spread throughout the body. It can infect the heart and cause inflamed coronary arteries and blood clots, as well as changes in blood pressure and heart rate. Approximately 75% of American adults have some form of gum disease - the majority unaware they have it as it is painless and silent in its early stages. The American Heart Association and the Centers for Disease Control recently urged doctors to test millions of Americans at moderate risk for heart disease for the presence of inflammation, mostly caused by chronic gum disease and urinary infections. Inflammation appears to be a trigger for heart trouble and to be even more dangerous than high cholesterol. The inflammation weakens blood vessels and makes fatty buildups burst. People with gum disease have twice the risk of dying from cardiovascular disease. By comparison, smokers only have a 60% increased risk. Nevertheless - DON'T brush your teeth for longer than two minutes. DO use floss at least once a day. DO visit your dentist at least once per year.
Dirty Teeth Can Kill You, US Study ShowsWashington - Germs found in dental plaque can make their way into the lungs and cause potentially fatal pneumonia in elderly nursing home patients, US researchers have reported. Though the study was small, the researchers said they found clear evidence in 8 patients who developed pneumonia while in the hospital that had originated from their own dental plaque. "This is the first study to establish unequivocally a link between dental hygiene and respiratory infection," said Dr Ali El-Solh of the University at Buffalo in New York, who led the study. Writing in the latest issue of the journal Chest, El-Solh and colleagues said they tested 49 nursing home residents who were admitted to a nearby hospital with a high risk of pneumonia. They made molecular fingerprints of the bacteria found in each patient's mouth before he or she developed pneumonia. Of the 49 patients, 28 had germs known to cause respiratory disease in their dental plaque samples and 21 did not. The patients were watched closely for pneumonia. The researchers said 14 eventually developed pneumonia and 10 of them had started out with respiratory disease-causing germs in their teeth. Tests of germs from the lungs showed the DNA matched the DNA of plaque germs in 8 of the patients - more than half. "These findings indicate that dental plaque is a reservoir of respiratory pathogens that can cause pneumonia in hospitalized institutionalized elders," said El-Solh. Nursing homes need to help patients maintain clean teeth and dentures, he added. Source: cnn.netscape.cnn.com 30 November 2004 © Reuters all rights reserved
Hot on the Trail of the Earwax GeneWhat Do Body Odour, Earwax and Breast Cancer Have in Common?by Mary Beckman That glop on the end of your Q-tip is more than just a sign of questionable hygiene, and now researchers are zeroing in on the gene that determines the consistency of earwax. Pinning down the gene's location could lead to a surprising range of advances - from curtailing body odor to predicting breast cancer. Earwax is made by apocrine glands that line the ear canal. Caucasians and people of African descent generally have "wet" earwax - a brown sticky goop - whereas Asians and native Americans usually have gray brittle flakes. The same glands in the armpit and genital region ooze an oily compound that ferments and provides a feast for stink-producing bacteria. In addition, breasts are giant modified apocrine glands. Too much apocrine tissue contributes to chronic breast cysts, and some researchers have proposed that a woman's earwax might contain clues about her risk of breast cancer. Researchers led by Norio Niikawa at the Nagasaki University School of Medicine in Japan first realised that they could pinpoint the earwax gene while studying a form of inherited epilepsy. Japanese families with the disorder had wet earwax - highly unusual in Asians. The team gathered DNA samples from nine families. By figuring out which bits of DNA were shared by those with sticky earwax, the researchers narrowed down the gene to a region on chromosome 16. They report the finding in the 8 June issue of The Lancet. Although that stretch of DNA could hold a couple hundred other genes, team geneticist Hiroaki Tomita predicts they will have the gene in hand within the year. Because wet earwax, body odor, and breast tissue seem to be related, the earwax gene "may control general apocrine gland development," he says. "I'm delighted they're close to finding the gene," says epidemiologist Nicholas Petrakis of the University of California, San Francisco. He says that the properties of apocrine glands - and therefore variety of earwax - corresponds to the risk of breast cancer. A genetic test could be more accurate than simply looking at earwax, which can be misclassified. Learning how the glands develop by studying the gene will help assess breast cancer risk in women, Petrakis says. Source: Daily InScight 7 June 2002 from Science magazine
For articles related to lifestyles including guns, television, extortion, hair, handbags, parenting, time bind, desserts, fitness, feasting, friends, happiness, ageing and more,
click the "Up" button below to take you to the Index for this Lifestyles section. |
 Animals
Animals Animation
Animation Art of Playing Cards
Art of Playing Cards Drugs
Drugs Education
Education Environment
Environment Flying
Flying History
History Humour
Humour Immigration
Immigration Info/Tech
Info/Tech Intellectual/Entertaining
Intellectual/Entertaining Lifestyles
Lifestyles Men
Men Money/Politics/Law
Money/Politics/Law New Jersey
New Jersey Odds and Oddities
Odds and Oddities Older & Under
Older & Under Photography
Photography Prisons
Prisons Relationships
Relationships Science
Science Social/Cultural
Social/Cultural Terrorism
Terrorism Wellington
Wellington Working
Working Zero Return Investment
Zero Return Investment